A sedentary lifestyle, injuries or excessive physical activity cause diseases of the musculoskeletal system. To avoid complications, it is important to start treatment early in the process. To do this, you need to know about the causes and symptoms of the pathology.
Description of the disease, what is its risk
Osteochondrosis of the thoracic spine is a chronic disease in which dystrophic changes begin in the cartilage located in the intervertebral space. The pathology is expressed by a decrease in the height of the discs and compression of the intercostal nerve endings.
Thoracic osteochondrosis goes through several stages of progression.
The first is characterized by the drying of the intervertebral disc, the decrease in stability and elasticity and the appearance of cracks. The pain is mild and goes away after the person gets some rest.
In the second stage, the disc decreases in height, the niche in the vertebra is filled with the nucleus pulposus, but does not go beyond its limits. Muscles experience constant tension. The person complains of severe pain, which goes away after resting.
The third stage is characterized by the protrusion of the nucleus pulposus beyond the edges, the crack reaches the vertebral end. As a result, an intervertebral hernia is formed. The pain becomes constant.
In the fourth stage, a proliferation of connective tissue is detected, which exerts pressure on the adjacent vertebrae. To compensate for the reduced layer, bone tissue begins to grow. More and more growths (osteophytes) appear.
Types of thoracic osteochondrosis and complications
Based on the nature of the pain, two types of thoracic osteochondrosis are distinguished:
- dorsago, which is characterized by acute sharp pain in the form of a lumbago, localized in the thoracic spine. The condition is accompanied by muscle tension, problems with movement in the neck and chest region;
- dorsalgia, in which the pain increases slowly. Inhalations and twists of the body, as well as prolonged standing in one position, add to the discomfort. At night, the discomfort deepens and disappears when walking.
In the absence of adequate therapy, the nerve endings are increasingly compressed. As a result, osteochondrosis of the thoracic spine can cause complications:
- diseases of the digestive system;
- persistent pain;
- interruption in cardiac activity;
- decreased ability to conceive;
- disturbance in the functioning of the lungs caused by the proliferation of connective tissue.
Why does the pathology of the thoracic spine occur?
This part of the spine experiences moderate load and limited mobility. However, the pathology is common. The disease can be caused by one of the reasons or by their combination:
- injuries and damages;
- excessive workload in the department, including in childhood;
- age-related changes associated with reduced nutrition of the disc tissue between the vertebrae;
- endocrinological diseases, especially during menopause;
- age-related impairment of calcium absorption;
- excess body weight;
- problems with blood vessels, atherosclerotic deposits in the vessels of the chest region;
- lean muscular corset.
How is the pathology manifested?
Symptoms of thoracic osteochondrosis include pain and increased muscle tone. The pain can be either short-lived with shooting or long-lasting pain. Pulling can be felt in the front of the chest, under the ribs and in the shoulder. The pain intensifies when you stay in one position for a long time.
A characteristic sign of the pathology is sensitivity to palpation of the spinous processes of the thoracic vertebrae.
The symptoms of osteochondrosis of the thoracic spine are similar to those of other diseases and include:
- discomfort in the heart area, reminiscent of angina pain;
- pain during breathing, shortness of breath, also manifested in pneumonia, tuberculosis, obstructive pulmonary disease;
- pain in the epigastric region, under the ribs, similar to the signs of gastrointestinal diseases.
Methods of treatment of thoracic osteochondrosis
If you have complaints, you should contact a neurologist. Therapy includes medication, physical therapy, exercise therapy, and massage.
Doctors prescribe medications:
- means to eliminate the source of inflammation in the back;
- medications to reduce muscle tone and the risk of compression of the sensory roots of the spinal cord;
- neuroprotectors designed to help restore nerve fibers.
The choice and dosage is chosen by the doctor, who will take into account the drug tolerance, accompanying pathologies and the patient's weight.
It is important to follow the recommended duration of treatment to avoid relapses. You can buy prescription drugs at a low price in the online store.
Massage should be done carefully, using friction techniques. The areas under the shoulder blades and between the ribs should be treated thoroughly. For the effect to appear, at least 10-15 sessions are needed.
During physical therapy, emphasis is placed on exercises that strengthen the muscular core, neck and lower back.
Ointments and gels with anti-inflammatory effects, heating patches and the Kuznetsov applicator are prescribed locally.
Osteochondrosis of the thoracic region
Osteochondrosis of the thoracic region is a degenerative pathology of the vertebrae and discs. Vlasenko Alexander Adolfovich (neurologist, doctor of manual therapy with 30 years of experience) talks about osteochondrosis of the thoracic region - symptoms, diagnosis and effective methods of treatment.
Why is thoracic osteochondrosis called a "chameleon"?
The thoracic spine has a special feature - the ribs are attached to it. Thanks to this, it is less mobile than the neck and lower back. Consequently, osteochondrosis in the chest region develops less often, according to the principle: "less mobility - less wear". But it develops less often - this does not mean that it continues more easily. And it really is. We are talking about chest pain. Since the area of thoracic back pain coincides with the area of the heart, the symptoms are often confused with angina pectoris or myocardial infarction. It is not for nothing that they say about thoracic osteochondrosis that it is a "chameleon". After all, he can claim not only that he has a heart disease, but also a disease of the lungs, liver, stomach, gall bladder or pancreas. And here you can not make a mistake and overlook a heart attack or other serious disease, for example, the pathology of the mammary glands in women. Such mistakes are costly, even if everything works out in the end. After all, this can "drive" a person into severe stress. That is why it is very important to find an experienced and knowledgeable doctor who will understand everything and distinguish the symptoms of thoracic osteochondrosis from other pathologies. Symptoms of osteochondrosis of the thoracic region are usually divided into two categories - radicular and reflex.
Symptoms of osteochondrosis
Manifestations of osteochondrosis will depend on the location and severity of the lesion in the spinal motion segment. In the initial stage, patients complain of dull, aching back pain, discomfort, slight limitation of movements in the spine, periodic numbness in the arms or legs, headaches and fatigue. By starting the treatment and changing the lifestyle during this period, the result will not be delayed and the recovery will come quickly.
With severe damage to the intervertebral disc, there is severe pain, persistent numbness and/or weakness in the arm or leg (depending on the level of damage). These signs can indicate the destruction of the intervertebral disc and the presence of a hernia, and it is necessary to immediately consult a doctor and start treatment.
In the most severe cases, the pain syndrome can be extremely severe, possible dysfunction of the pelvic organs, severe weakness and numbness in the arm or leg. If these signs are present, urgent hospitalization is necessary to resolve the issue of surgical treatment.
With cervical osteochondrosis, pain appears in the neck, may radiate to the shoulder, arm or head, numbness or weakness in the arm, headache, dizziness.
With osteochondrosis of the thoracic spine, pain appears in the chest, radiates to the sternum or scapula, intensifies with breathing and movement, and sometimes there is a feeling of shortness of breath. Patients often confuse this condition with heart pain.
When the lumbosacral spine is affected, the pain is localized in the lower back, intensifies with movement, radiates to the legs or perineum, and numbness or weakness in the legs may appear.
It is necessary to remember that our body is a single whole, and the division of osteochondrosis into cervical, thoracic and lumbar is arbitrary. As a rule, the disease develops in the entire spine, but it manifests itself in the part that experiences the greatest load.
Radicular symptoms
They occur due to the impact on the nerves that leave the spine.
Spinal nerves
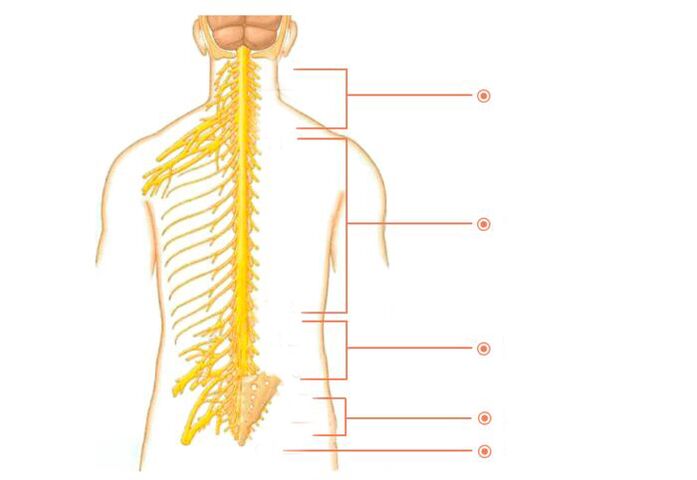
There are many nerves that come out of the spine. They are called spinal nerves. Each such nerve gradually branches out and follows a specific area of the body with clearly defined boundaries. This area is called the area of segmental innervation. Each vertebra, disc, nerve and area is numbered, corresponding strictly to each other. If a nerve is exposed, the symptoms will appear in the area of segmental innervation corresponding to that nerve, and not everywhere - in an arbitrary place.
Radical symptoms include:
- Decreased or lost reflexes;
- Impaired sensitivity;
- Muscle weakness;
- Radicular pain.
Areas of innervation of the thoracic segments
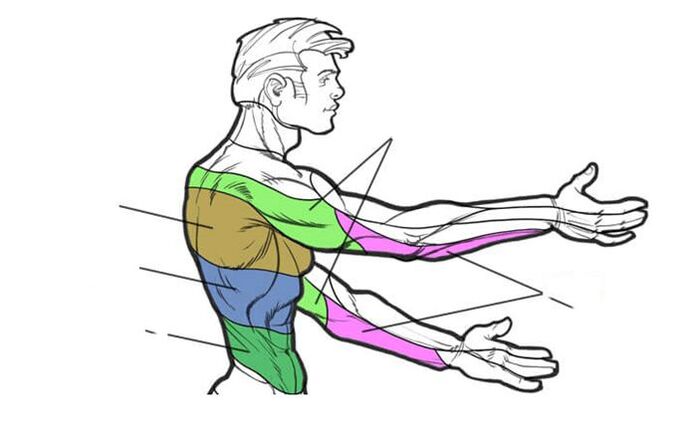
Osteochondrosis D1-D2– Causes pain in the shoulder, collarbone and armpit areas.
Osteochondrosis D3-D6- causes pain of generational character in the upper part of the chest. Simulates heart pain, an angina attack. In women, it causes pain in the mammary glands.
Osteochondrosis D7-D8- causes belt pain at the level of the solar plexus. Simulates pain in the stomach, liver, gall bladder or pancreas. Reduces upper abdominal reflexes.
Osteochondrosis D9-D10- causes pain in the hypochondrium and upper abdomen. Sometimes it imitates the so-called "acute" abdomen - sharp pains in the abdomen. Reduces mid-abdominal reflexes.
Osteochondrosis D11-D12- causes pain in the hip area. Simulates pain in women's diseases, appendicitis and intestinal diseases. Reduces lower abdominal reflexes.
Reflex symptoms
Unlike radicular symptoms, reflex symptoms do not have clear boundaries. These can be: difficulty breathing, lack of air, pain during inhalation and exhalation, chills and "bumps" on the skin, intercostal neuralgia, chest pain in the waist. Indigestion is often observed - appetite worsens, nausea, heartburn, bloating and bowel dysfunction appear. Because of the pain, sleep is disturbed, insomnia appears and the feeling of not getting enough sleep appears. It is difficult to move, especially in the morning. Coordination of movements is impaired - this is reflected in walking. General weakness, weakness. Sexual disorders. Nervousness. Rapid fatigue. Various pains appear. Pressing pain in the chest area. Pain between shoulder blades. Pain in the hypochondrium. Pain when raising the arms. Pain when you bend over or try to stand up. Pain between shoulder blades. In general, pain in osteochondrosis of the chest region is usually divided into two types.
Dorsalgia- moderately strong, prolonged pain in the back and chest with periods of intensification and weakening.
Dorsago- acute painful "lumbago" in this area.
- Symptoms of osteochondrosis of the chest region depend on the stage of osteochondrosis.
- They get worse when you bend over or try to stand up.
- Symptoms often appear after 35-45 years.
- They appear approximately 3 times more often in women than in men.
You have, of course, noticed that the radicular symptoms are quite clearly defined, while the reflex symptoms are very vague and non-specific. And as you know, everything that does not have clear definitions serves as a convenient cover for professional helplessness. This applies, among other things, to reflex symptoms and such a favorite concept of doctors as "age-related changes". Surely many of you are familiar with the situation when the doctor explained the problem as "reflex" or "age-related" processes. Most people at such moments rightly believe that the doctor simply cannot understand what is happening and is trying to hide his incompetence in the fog of these "magic words".
At one time there was a popular phrase: "Every accident has a name, a surname and a position. "So each disease has its own unique symptoms. And it is the doctor's duty to recognize them clearly. And then there will be no need to cast a fog and blame osteochondrosis of the thoracic region for everything. Now you understand how important it is to find an experienced and knowledgeable doctor. Correct diagnosis and good treatment results will depend on this.
Stages of the disease
| phase | Changes | Symptoms |
| First | Dehydration of the discs, which causes loss of elasticity. Their height decreases, but their width increases - the intervertebral disc gradually flattens. | The pain appears directly in the damaged ring. It can be pull or throw. |
| Secondly | The annulus fibrosus begins to disintegrate. The nerve roots are compressed, causing pain. | There is pain during movement. When you hold a pose for a long time, discomfort appears. |
| Third | The annulus fibrosus ruptures, causing a herniated disc to form. Pathological scoliosis or kyphosis develops. | There is pain during movement. When you hold a pose for a long time, discomfort appears. |
| Fourthly | The vertebrae rub against each other, which provokes the displacement of the intervertebral joints. The tissues surrounding the vertebrae become inflamed. Cartilage tissue is replaced by bone tissue, which reduces motor functions. Fibrosis appears. | There is pain during movement. When you hold a pose for a long time, discomfort appears. |
Phases of exacerbation and remission may be observed. The latter is often observed in stage 4.
Disease rates
This is a more modern classification of symptoms of thoracic osteochondrosis, which is used by specialists.
| Diplomas | Changes and symptoms |
| First | Fracture of the intervertebral disc caused by sudden movements or overexertion. Sharp pain, similar to the passage of electric current along the spine. Muscle strain. |
| Secondly | It is characterized by instability of the spine. Pain during movement. Extension. |
| Third | The pain becomes constant. Loss of sensitivity. Change in gait. Severe headaches. Difficulty in breathing. Tachycardia. |
| Fourthly | The spine is unstable: the vertebrae slip and twist. Osteophytes grow, compressing spinal nerves and putting pressure on the spinal cord. |
Thoracic osteochondrosis can cause serious diseases that will be difficult to cure.
Diagnosis is the key to proper treatment
Today, there are a number of modern methods for the hardware diagnosis of osteochondrosis. The most accurate of them are MRI and CT. But the main method is still clinical diagnosis - this is when an experienced doctor compares data from at least three sources - from the patient's complaints, MRI results and symptoms that were identified during the examination. This allows you to make a diagnosis as accurate as possible and create an effective individual treatment program.
Who to contact, methods of examination of osteochondrosis
As a rule, with back pain, patients are referred to a neurologist, who, based on complaints and a neurological examination, can make a preliminary diagnosis, prescribe additional examination methods (x-rays of the spine, MRI, CT, analysis ofgeneral urine test, general blood test) and develop a treatment regimen.
Treatment
Treatment should be comprehensive, aiming to:
- elimination of pain syndrome;
- elimination of damaged function of spinal roots;
- preventing the progression of degenerative-dystrophic changes in the structures of the spine.
During the acute period, with severe paindrug treatment is prescribed: Non-steroidal anti-inflammatory drugs, muscle relaxants, B vitamins, chondroprotectors or blockades are used.
Physiotherapyis the main method of conservative treatment of diseases of the musculoskeletal system. Exercise therapy is aimed at forming, correcting and strengthening the muscle corset; increased range of motion in the back and joints; development of a motor stereotype and correct posture; reducing the load on the spine.
With regular exercise therapy, joint exercises, yoga or swimming, blood supply and tissue nutrition are improved, metabolism is normalized and the intervertebral space is increased, which leads to recovery.
Listen to your body, if you find symptoms of osteochondrosis or your lifestyle includes prolonged sitting at the computer, driving a car or insufficient physical activity, seek help from a specialist without waiting for deterioration.
As you understand, osteochondrosis is a real "mess" of symptoms, which, unraveling, the doctor will free you from pain and suffering. But it is not possible to eliminate changes in vertebrae and discs. Therefore, the words "treatment of osteochondrosis" must be understood correctly. If you are interested in eliminating pain and other suffering, then yes, it is quite possible. And if you conduct an academic discussion on the subject of returning vertebrae and discs to their original appearance, "like a newborn baby", then no, the past cannot be returned. You have to be realistic and then you won't fall for scammers.
Which treatment method is considered the main one?
Gentle manual therapy is the main type of treatment for osteochondrosis of the thoracic region. It's like an antibiotic for pneumonia - you can't do without it. The remaining types - massage, medications, physiotherapy and exercise therapy - are supportive.
Physiotherapy
Physiotherapy methods relieve swelling and inflammation, improve blood circulation in the affected area, reduce or stop pain.
Magnetic laser, magnetotherapy, SMT with novocaine, ultrasound with hydrocortisone, etc.
Balneotherapy: Mud applications, ozokerite applications in affected areas, radon baths.
Exercise therapy and massage
Therapeutic exercise is the main method of treatment of osteochondrosis. Gymnastics is performed regularly for 10-15 minutes several times a day. To increase effectiveness, a massage course is prescribed. The procedures help to relax the muscles, reduce pressure on the vertebrae, improve metabolic processes and blood flow. Exercise therapy can be performed independently at home, also in the clinic (individual and group classes). Massage is performed by a qualified specialist in a clinical setting.
How does gentle manual therapy work?
The nutrition of the discs is directly related to the muscles that surround the spine. In addition, the back muscles themselves are one of the component causes of pain in osteochondrosis of the thoracic region. Gentle manual therapy is a special method that allows you to return muscles to their natural physiology, eliminate spasms, muscle tension and improve disc nutrition.
The intervertebral discs are the only part of the body that does not have blood vessels and is nourished by the proper functioning of the muscles.
In addition, while performing the treatment using the hands, the chiropractor:
- will relieve the load from the affected vertebrae and discs and distribute it correctly;
- relaxes muscles and helps them return to normal;
- relieves the patient from the clamps;
- improving the power supply of the disk;
- will restore the motor functions of the body;
- normalizes blood circulation.
Manual impact mobilizes the body's internal forces and promotes self-healing mechanisms.
Acupuncture
The technique consists in influencing the biologically active points of the body with thin needles. The procedure reduces the manifestation of pain and inflammatory processes. Acupuncture is not painful and there may be minor discomfort.
Treatment of pathology in women
It is practically impossible to completely get rid of thoracic osteochondrosis already in progress, but it is quite possible to slow down or even stop the formation of a degenerative-dystrophic pathological process in the tissues of the spinal movement segments using the tools and methods of modern medicine. . The optimal therapeutic effect can be achieved only with an integrated approach to the treatment of this pathology using medications, various physiotherapeutic techniques and targeted exercise therapy techniques (physical therapy).
Symptoms and treatment of osteochondrosis of the thoracic spine in women are not much different from those in men. In the acute period of osteochondrosis of the thoracic segment of the spine, the patient needs intensive treatment of the deterioration, during which various medications and physical procedures are used to help eliminate, first of all, the pain syndrome and in parallel with other manifestationsnegative. of the disease.
During remission, the patient should be prescribed maintenance treatment, mainly based on taking drugs that restore the osteochondral structure and physical therapy. In particularly severe cases, they sometimes use surgical intervention to stabilize the position of the spine.
What should you do in case of deterioration?
During an exacerbation, severe pain appears, radiating along the intercostal space. At this stage, it is necessary to maintain bed rest and reduce the mobility of the spine. Symptoms are eliminated with analgesics prescribed by the attending physician.
The treatment is absolutely safe.
Preventing
To prevent the disease and slow down the degenerative processes, it is recommended:
- weight regulation;
- cycling, running, swimming, yoga and other sports;
- daily walks;
- taking vitamin complexes and chondroprotectors;
- reducing stress on the back;
- timely treatment of musculoskeletal diseases.
To avoid relapses, create comfortable conditions for sleeping and working. Watch your weight and eat right. Continue your physical activity. But the main thing is not to neglect your health and do not save on it. Don't let things take their course. After recovery, try to do at least one maintenance session of gentle manual therapy once every three to six months - this will reduce risk factors. Remember, advanced osteochondrosis leads to complications - disc protrusion and herniation. Remember: your health comes first!



















