Back pain is quite common. It can be caused by both ordinary fatigue and serious injuries and pathologies. If the pain is severe or does not go away after rest, it is important to consult a doctor to rule out dangerous conditions.
What can lower back pain be like?
Pain in the lower back can be sharp or aching, appear suddenly or increase gradually, appear with certain loads or movements (for example, bending over) or continue regardless of what the person is doing.
The pain may be point-like or radiating (ie, spread to other areas). In this case, a person has pain not only in the back in the lumbar region, but also in other parts of the body, such as at the bottom of the abdomen, perineum, legs or buttocks.
Back pain may include stiffness of movement or muscle spasms. The person may have difficulty bending over or rising from a lying position, standing with their back straight, or maintaining a posture when walking.
If the pain is caused by a muscle spasm or a pinched nerve, it can be excruciating and even incapacitating. Such pain forces you to stay in bed until you get medical help.
Why does my lower back hurt?
The most common cause of pain in the lower back is one or another pathology of the musculoskeletal system: sprains, strains, inflammations. They are often found in men who work with their hands, athletes and new mothers.
Also, discomfort in the lower back can be a sign of acute or chronic diseases of the internal organs. This happens due to the fact that pain impulses are able to be transmitted along nerve fibers to neighboring regions. In this case, they say that the pain "radiates" to the lower back.
Diseases of the musculoskeletal system that cause pain in the lower back
Most often, back pain is caused by injuries and pathologies of the musculoskeletal system - sprains of muscles and ligaments, spinal cord injuries, hernia and protrusion of intervertebral discs, joint inflammation, bone diseases.
Deformations and sprains of muscles and ligaments
Such injuries can occur due to awkward movement if a person lifts something too heavy or does not follow safety precautions when handling heavy objects. You can also get hurt while playing sports or if you just sneeze unsuccessfully.

Lower back pain can occur if you lift heavy objects without following safety precautions.
With sprains and strains, pain intensifies during movement and muscle spasms may occur. It may be painful for the person to walk, bend forward, or keep their back straight.
The diagnosis of deformation and sprain of muscles and ligaments is based on data from a physical examination and instrumental studies - ultrasound, x-ray, MRI of the lumbar region. If you suspect a sprain or deformation of muscles or ligaments, you should contact an orthopedic traumatologist.
Treatment consists of relieving acute pain and muscle spasms using ice packs, pain relievers, and medications to relieve muscle spasms (muscle relaxants). It is important to rest the injured area to allow the tissue to recover - this usually takes around 2 weeks. After that, it is important to start rehabilitation: physical therapy exercises aimed at restoring muscle function are indicated.
Without treatment, strains and sprains lead to limited mobility: trying not to injure the injured area, a person reduces activity, which can lead to weight gain, decreased bone strength, and loss of muscle mass.
Spinal cord injuries
Damage (usually a fracture) to one or more vertebrae occurs as a result of falls, accidents, sports or household injuries. In people with bone density disorders (such as osteoporosis), such damage can be caused by even small exposures.
The treatment of spinal injuries is to prevent further displacement and deformation of the spinal discs. If the injury is not severe, it is recommended to sleep on a hard surface and limit physical activity. If the damage is significant, surgical methods are used for fixation.
Without treatment, damage to the spinal discs can cause stenosis (narrowing) of the spinal canal, neurological disorders, including sciatica - pinched nerve fibers that extend from the spine.
Pathologies of intervertebral discs
Intervertebral discs are fibrocartilaginous plates with jelly-like contents located between the vertebrae. They act as absorbent cushions for the vertebrae, ensuring their mobility. Discs can be displaced (prolapsed) or ruptured (herniated), causing severe pain and limiting the mobility of the spine.
Intervertebral hernias and protrusions can occur in people with weak muscles and excess weight, in those who lead a sedentary lifestyle or who lift heavy objects. People who smoke are more susceptible to intervertebral disc pathologies.

Intervertebral hernia - protrusion of an intervertebral disc into the spinal canal
Treatment consists of relieving pain and inflammation – rest, painkillers, ointments and compresses in the inflamed area are recommended. The doctor may prescribe physical therapy or exercise therapy. For moderate injuries, the disc can heal if the cause of the herniation or protrusion is ruled out - for example, strengthening the muscle corset, reducing weight and not putting too much stress on the spine.
If the pain in the lower back is so strong that it interferes with daily activities, does not go away within 1-1. 5 months, or if the symptoms worsen, you should contact your doctor again. In some cases, steroid therapy or even surgery may be required. With age, it is possible to develop a degenerative disease of the intervertebral discs - they become flatter and perform a worse shock-absorbing function, which can also cause pain. In this case, treatment includes pain relief and general improvement of the body.
Scoliosis of the lumbar spine
Scoliosis (curvature) of the spine is a displacement of the spine to the right or left in relation to the vertical axis. The pathology leads to increased pressure in certain areas of the intervertebral discs and vertebrae, as well as in compressed tissues and nerve fibers. Scoliosis can cause severe pain in the lower back on the right or left side - where most of the stress is placed - and severely limit the mobility of the spine.

Scoliosis (curvature) of the spine can cause severe pain in the lower back where a lot of stress is placed
Scoliosis can occur due to the weakening of the muscle belt in the absence of sufficient physical activity, a sedentary lifestyle (in schoolchildren, office workers). In this case, it is difficult for the muscles to maintain the physiological position of the back and curvatures are formed.
Treatment includes the introduction of balanced physical activity (physiotherapy, swimming), massage and manual therapy, physiotherapeutic procedures for muscle strengthening, such as electrical stimulation. For severe injuries, wearing a corset is recommended, which helps maintain the correct position of the spine.
Arthritis and arthrosis
Inflammation and degenerative processes in the joints of the spine can also cause severe back pain. There are many forms of arthritis, including osteoarthritis (damage to cartilage and adjacent tissues), ankylosing spondylitis (ankylosing spondylitis - damage to the joints of the spine, leading to fusion of the vertebrae).
Arthritis can be caused by natural aging, genetic predisposition or autoimmune disease.
Arthritis treatment, depending on its form, may include the use of non-steroidal and steroidal anti-inflammatories and sedatives, physiotherapeutic procedures (magnetic therapy, electrophoresis), therapeutic massage and physical therapy.

Physiotherapy procedures help relieve pain due to joint pathologies
Spondylolisthesis
Displacement of a vertebra in relation to the spine (spondylolisthesis) occurs as a result of injury or degenerative processes in the spine. Pathology appears in athletes, elderly people or people with a hereditary predisposition to bone diseases (for example, osteoporosis - a disorder of bone density). Spondylolisthesis can lead to severe pain in the lower back, buttocks and legs and cause leg cramps or weakness.
Treatment involves relieving pain and inflammation that occurs due to compression of adjacent tissues by the vertebra. Depending on the severity of the pain syndrome, the doctor may prescribe non-hormonal painkillers in tablets or injections of corticosteroid drugs. At the same time, physiotherapeutic procedures and exercise therapy are prescribed to strengthen the muscles and restore the position of the vertebrae. If spondylolisthesis is accompanied by severe pain, surgical treatment is used.
In traumatic and non-infectious pathologies of the musculoskeletal system, the pain in the lower back usually decreases or decreases when the person takes a comfortable position.

If spondylolisthesis is accompanied by severe pain, your doctor may prescribe corticosteroid injections.
Infectious diseases of the spine
Inflammation of the bone tissue (osteomyelitis) and inflammation of the intervertebral disc (discitis) can cause severe back pain. These pathologies, as a rule, are of a secondary nature, that is, they arise as a complication of inflammation of other organs (the infection enters the tissues through the bloodstream).
Treatment involves hospitalization, lasts up to 1 month, and then requires rehabilitation, which lasts from 6 to 12 months.
Tumor diseases of the spine
Neoplasms can develop under the influence of hereditary or external factors (for example, radiation), but more often they appear as repeated foci (metastases) in cancer of other organs - lungs, mammary glands, prostate, thyroid gland, kidneys.
One of the most characteristic symptoms of tumoral pathologies is pain that does not subside during a change of position or after rest. Symptoms such as numbness, partial paralysis, uncontrolled urination and a sharp increase in body temperature with chills are also possible. Without treatment, symptoms worsen.
Treatment is prescribed depending on the type of tumor, its location and symptoms and may include chemotherapy, radiotherapy and surgical removal of tumors. Pain relief is carried out with non-hormonal or steroid drugs. To stabilize the spine, your doctor may prescribe wearing a brace.

Orthopedic corset helps to stabilize the spine
Diseases of internal organs that cause pain in the lower back
Back pain can occur with diseases that are not associated with pathology of the spine and adjacent tissues. Acute or painful, it can accompany inflammation of internal organs: pyelonephritis, urolithiasis, aneurysm of the abdominal aorta. In women, pain in the lower back can develop due to gynecological pathologies.
Urolithiasis disease
A disease in which stones are formed in the kidneys and bladder - hard formations from the sediment of chemical components of urine. Back pain is one of the main signs of pathology. Depending on the size and location, kidney stones can cause a dull, aching pain that appears and subsides periodically, or a very sharp pain that does not go away on its own and requires urgent medical attention.
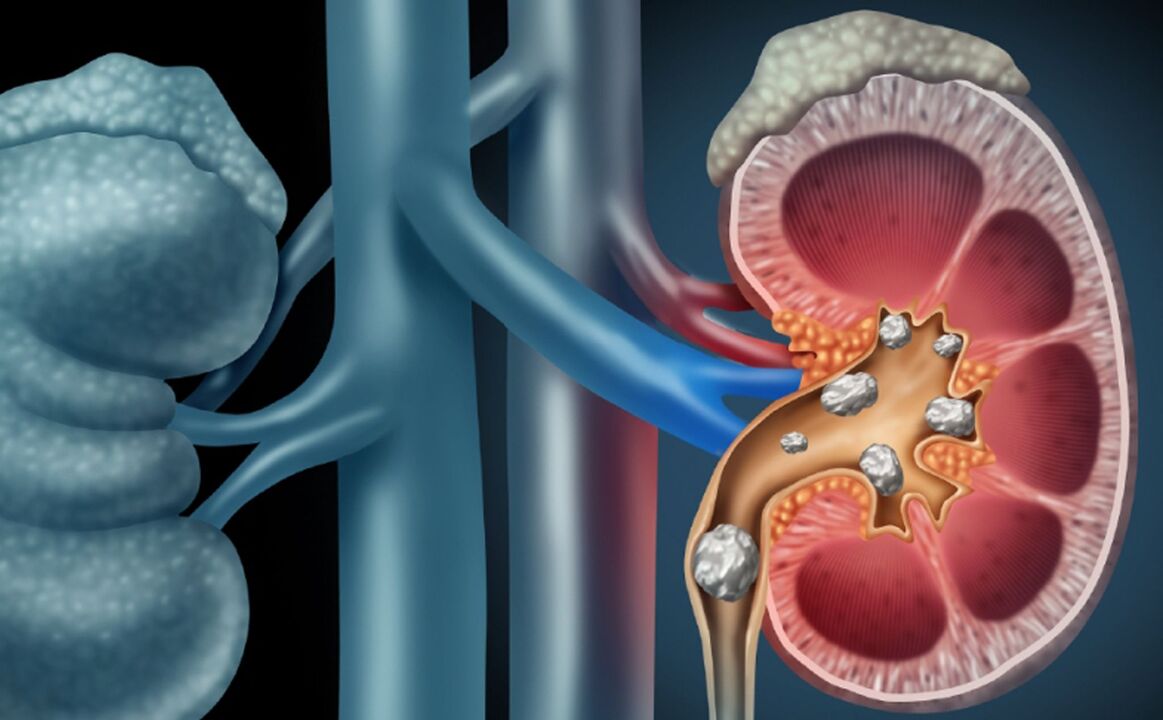
Urolithiasis - the formation of stones in the kidneys and bladder
If you suspect kidney stones, you should contact a urologist or nephrologist. The doctor will prescribe tests and instrumental studies (ultrasound, X-ray examination, computed tomography, including the use of a contrast agent) to make a diagnosis and choose treatment tactics.
Treatment is prescribed taking into account the size, nature, location of the stones and other factors. If the stone is small (5-10 mm) and there are no other indications for surgical removal, drug treatment is used. If within a month there are no positive dynamics, removal by non-invasive or surgical methods is recommended.
Aneurysm of the abdominal aorta
Weakening of the walls of the abdominal aorta (aneurysm) can lead to life-threatening conditions such as aortic rupture and intra-abdominal bleeding. As a rule, the pathology appears in the elderly: the risk group includes men over 65 and women over 70, including smokers, those suffering from vascular disease (high blood pressure), who have previously had aneurysms or hadhereditary predisposition to them.
Lower back pain due to an abdominal aortic aneurysm does not subside over time and may be accompanied by abdominal and leg pain.
If an aneurysm is suspected, an abdominal ultrasound and computed tomography are prescribed.
Treatment depends on the size of the aneurysm. Small changes require monitoring with twice-yearly instrumental examination and lifestyle adjustments. Significant (over 5 cm, with high risk of rupture) are an indication for abdominal or minimally invasive surgery.
How to prevent back pain
Since back pain is most often caused by traumatic injuries to muscles, fascia, joints or bones, the main recommendation for prevention is to follow safety precautions, maintain a strong muscle core, and healthy bones and joints.
Prevention of sprains and microtraumas of the lower back:
- a varied diet that includes the vitamins and minerals needed to keep bones and muscle tissue and joints healthy;
- maintaining a healthy weight;
- regular physical activity: exercises to prevent back pain should include strength exercises to develop the muscular frame, stretching to relieve muscle tension and spasms, and cardio training to maintain blood supply and tissue nutrition;
- observing safety precautions when playing sports - for example, the first classes in the gym must be supervised by a qualified trainer;
- compliance with safety precautions at home - many injuries can be avoided if you wear comfortable shoes, keep the railings on the stairs, take the time when it is slippery outside;
- observing safety precautions when lifting heavy objects - the load on the spine will be less if you approach the object as close as possible (do not grab it), and when lifting objects from the floor, bend your legsinstead of tilting the body.

Yoga and pilates classes help relieve spasms and tension in the lower back
Smoking impairs blood circulation and impairs tissue nutrition, increasing the risk of damage and injury.
What to do if your lower back hurts
If your lower back hurts, the reasons may be different, which means that the treatment tactics will also be different.
In case of severe physical fatigue, the back should be given a rest - perhaps this will be enough for the muscles to recover and the mobility of the spine to return.
If the pain does not go away within 1-2 days or if it is very strong, you should consult a doctor. While you wait for a doctor, you can try to relieve acute pain with pain relievers.
At the appointment, the doctor will perform an examination, determine the cause of the pain and give recommendations for treatment. This will help to eliminate dangerous conditions and prevent the development of complications.
Heating (lumbar roll, hot water bottle, sauna) is contraindicated for inflammation, but can relieve acute pain in the lower back if it is caused by muscle fatigue or a pinched nerve. These methods can be used only after consulting a doctor.
Which doctor should I contact for a complaint of lower back pain?
If you suspect pathology of the musculoskeletal system, you should contact a neurologist and orthopedic traumatologist.
The diagnosis is carried out during a physical examination and using instrumental methods: magnetic resonance therapy, computed tomography, X-ray and ultrasound. It is also possible to prescribe a myelogram (X-ray or CT study with a contrast agent injected into the spinal canal) and electromyography - a study that allows you to assess the condition of nerve and muscle fibers.
If you suspect kidney disease, you should contact a urologist, nephrologist or therapist. The doctor will analyze the complaints and perform a physical examination, and then prescribe laboratory and instrumental tests to clarify the diagnosis.
Based on blood and urine tests, the doctor will be able to determine if there is inflammation in the organs of the urinary system, and ultrasound and x-ray studies will help visualize the organs, determine the cause of the pain and choose the best treatment. effective. tactics.
If the origin of lower back pain is unclear, you should consult a general practitioner or therapist.
The doctor will collect an anamnesis (medical history), analyze hereditary risks, perform a physical examination and prescribe tests that will identify inflammatory processes or disorders in the functioning of internal organs.
A general blood test helps to identify the inflammatory process.
If necessary, the doctor will refer you for instrumental studies (ultrasound, X-ray, MRI) or will recommend you to contact a specialist for diagnosis and further treatment.



















